The quest for understanding ovarian cancer has taken a significant turn thanks to groundbreaking research focused on the cellular origins of the most prevalent and aggressive variant, high-grade serous ovarian carcinoma (HGSOC). Recent studies conducted on mouse models have unveiled critical insights into the oviducts—the structures that precede the ovaries and act as conduits for eggs. These findings, if applicable to humans, might pave the way for early detection methods that could dramatically improve patient outcomes. Historically, the prognosis for HGSOC has been grim, with a survival rate indicating that the majority of patients succumb within five years post-detection.
Origins of Ovarian Cancer: A Paradigm Shift
For over a decade, researchers have gradually shifted their focus from the ovaries themselves to the fallopian tubes, where mounting evidence suggests that many ovarian cancers may initiate. Investigations into these structures have revealed genetic lesions at the ends of the fallopian tubes that correspond to tumors found in the ovaries. Despite these efforts, the specific types of cells responsible for HGSOC within the fallopian tubes remained largely unidentified, limiting the development of efficient diagnostic and therapeutic strategies.
A common hurdle in diagnosing HGSOC lies in the subtlety of its early symptoms, often leading to late-stage detection when treatment becomes significantly more challenging. Current statistics indicate that roughly 80 percent of cases are diagnosed at advanced stages, underscoring the urgency of improving early detection mechanisms. The team led by Cornell University’s pathologist Alexander Nikitin highlights that understanding the cellular landscape of the oviduct can be pivotal in unveiling new biomarkers for diagnosis, as well as potential therapeutic targets.
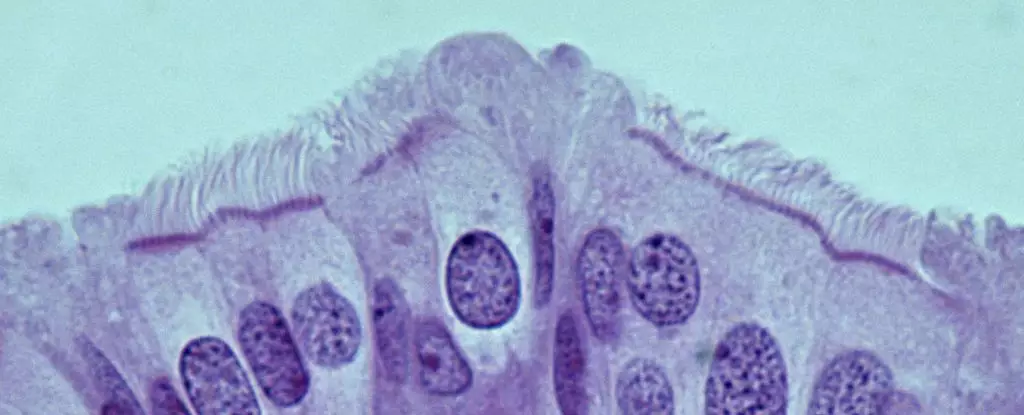
In a pivotal study published recently, Nikitin and his collaborators identified specific stem cells in the ovaries linked to HGSOC. However, their latest findings, which focus on the oviducts in mice, reveal previously uncharted territory: the characterization of all cell types present in the oviduct for the first time, shedding light on potential cancer-prone cells. Surprisingly, the primary cell type contributing to cancer susceptibility was not the expected stem cells but rather pre-ciliated cells—transitional cells poised to develop into ciliated cells that facilitate the movement of oocytes through the reproductive tract.
This critical differentiation emphasizes the need for deeper exploration into the role of these transitional cells in cancer initiation. The study’s results show that certain genetic mutations typically associated with HGSOC disrupt the normal functioning of pre-ciliated cells, leading to enhanced cancer formation. This suggests a compelling relationship between cilia formation—an essential biological process for cellular function—and the pathogenesis of ovarian cancer.
As researchers delve deeper into the findings of this study, the implications of identifying the precise cells involved in HGSOC could be profound. The link established between ciliogenesis irregularities and ovarian cancer raises a beacon of hope for future investigations. Additionally, the fact that similar issues with ciliogenesis have been observed in pancreatic cancer could indicate broader ramifications in our understanding of how certain cellular processes may transcend different cancer types. Further studies are vital to unravel the complexities behind tumor formation, looking at whether other genetic mutations linked to HGSOC exert comparable influences on cancer development.
The commitment to enhance early detection and treatment strategies could have life-saving consequences for many women. As this field of research continues to advance, it not only holds the promise of identifying new diagnostic markers but also fosters the potential for tailored therapies that directly target the mechanisms of initiation associated with HGSOC. Ultimately, a heightened understanding of the cellular underpinnings of ovarian cancer may significantly influence patient survival rates and quality of life in the years to come.