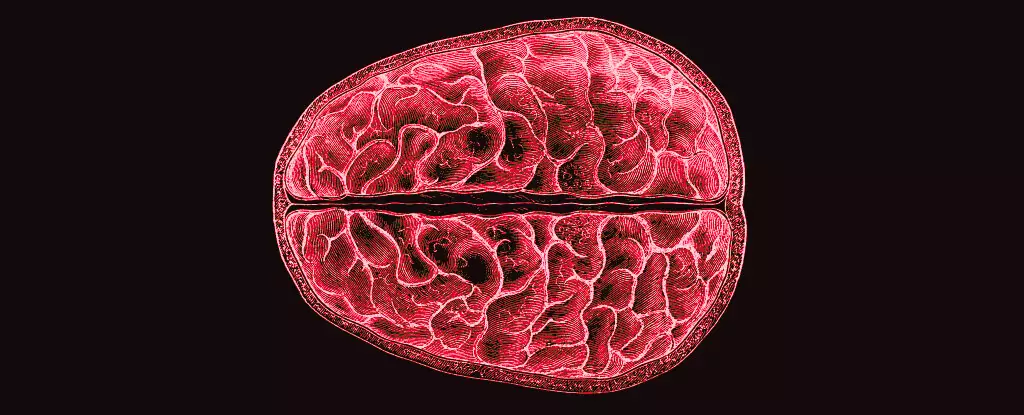
The menstrual cycle is a physiological phenomenon that has captivated scientists for centuries, yet its implications extend far beyond reproductive health. Recent research conducted by neuroscientists at the University of California Santa Barbara has unveiled the profound influence of hormonal fluctuations during the menstrual cycle on the brain’s structure itself. This groundbreaking study not only contributes to our understanding of women’s health but also suggests that these hormonal rhythms could have broader implications for cognitive function and mental health, an area that has been notably underexplored.
Led by Elizabeth Rizor and Viktoriya Babenko, the research team investigated a cohort of 30 women over the course of their menstrual cycles, using advanced imaging techniques to capture the brain’s changing landscape. Unlike previous studies that focused primarily on cognitive tasks or behavior, this research meticulously mapped structural changes, including microstructure variations in white matter and cortical thickness associated with hormonal fluctuations. The researchers highlighted a significant finding: the interaction between hormones and brain structure is not confined to traditionally recognized areas of the brain, suggesting a more complex relationship than previously understood.
The brain’s plasticity—a term denoting its ability to reorganize itself—has been a key focus in neuroscience. This study underscores how menstrual hormones can induce changes not just functionally but also structurally, which adds a new dimension to our understanding of brain health. For instance, white matter, which acts as the brain’s information superhighway, appears to undergo transformations in response to hormonal shifts. The study documented these variations during three distinct phases of the menstrual cycle: the menstrual phase, ovulation, and mid-luteal phase, offering insights into the timing and nature of these changes.
One striking observation from the research is the correlation between heightened levels of 17β-estradiol and luteinizing hormone leading up to ovulation and observable alterations in white matter. These changes indicate enhanced information processing capabilities, potentially suggesting that cognitive functions could be more pronounced at certain times of the cycle. In contrast, the surge in follicle-stimulating hormone was linked with increased thickness of gray matter, which serves as an essential brain region responsible for processing sensory information and executing motor functions.
Additionally, the research indicated that progesterone, which ascends post-ovulation, was associated with increased brain tissue volume and a decrease in cerebrospinal fluid. While the precise implications of these changes remain to be elucidated, such fluctuations may influence emotional responses and cognitive capabilities, further intricately tying mood dysregulation and mental health challenges to the menstrual cycle.
Despite these compelling findings, the broader implications of hormone-driven brain changes are yet to be fully understood. While this study paves the way for future inquiries into how these modifications might affect cognitive behaviors, emotional states, and overall mental well-being, the scientific community has a pressing responsibility to continue exploring these connections.
Research on the menstrual cycle has historically lagged, often overshadowed by investigations centered on male physiology and hormonal functions. The resulting knowledge gap begs the question: why has it taken so long for women’s health to be prioritized in scientific research? Addressing these issues can lead to innovative therapies and strategies for managing period-related mental health challenges—an area recognized but not fully understood.
The intricate dance of hormones throughout a woman’s menstrual cycle does not merely pertain to reproduction—it profoundly shapes neurological frameworks and cognitive abilities. As we unravel the complexities of these hormonal influences, we can better understand the full spectrum of women’s health, paving the way for informed mental health interventions and innovative bedrock research aimed at the different life stages of menstruating individuals. This study should inspire a renewed focus on menstrual health—not just as a biological process, but as a pivotal element of overall cognitive and emotional wellness. The future of women’s health research is ripe for exploration, and this study serves as a vital stepping stone toward deeper understanding.