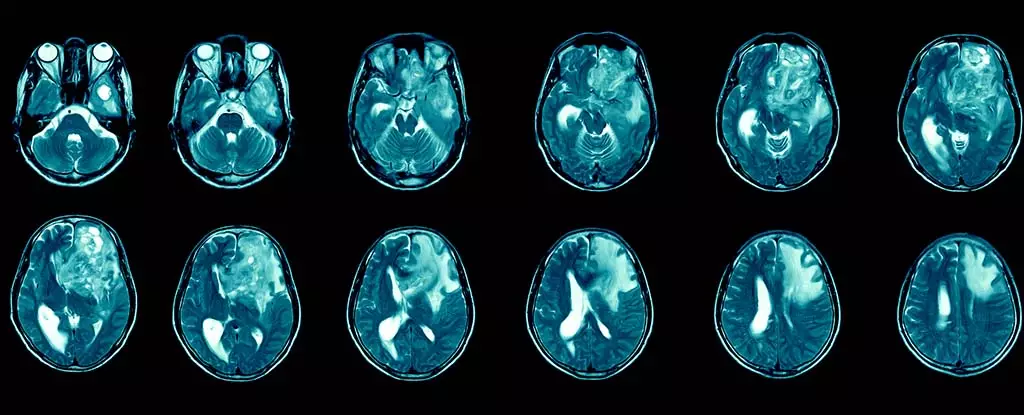
Glioblastoma, classified as a grade 4 tumor by the World Health Organization, is recognized as both the most prevalent and lethal variety of brain cancer. Patients diagnosed with glioblastoma face an incredibly grim outlook; the average survival time is alarmingly short, at just 12 to 15 months post-diagnosis. Furthermore, a mere 6.9% of those afflicted manage to survive beyond the five-year mark. These statistics paint a stark picture of a disease that continues to elude effective treatment strategies. Beyond sheer survival rates, glioblastoma inflicts a cruel toll on patients’ lives, manifesting through debilitating symptoms such as persistent headaches, unpredictable seizures, profound cognitive shifts, and dramatic changes in personality. These issues severely degrade the quality of life, affecting not only the patients but their families and caregivers as well.
This aggressive cancer is part of a broader classification known as gliomas, which are tumors that originate within the brain and spinal cord. In the United Kingdom alone, there are approximately 3,200 new cases diagnosed annually, which contributes significantly to the total of 12,700 brain and central nervous system tumor cases reported each year. Globally, the incidence rate ranges between 3.2 to 4.2 cases per 100,000 people, leading to an estimated total of 150,000 new cases worldwide each year. This underscores the pressing need for effective therapeutic interventions.
Conventional treatment approaches—surgery, radiation therapy, and chemotherapeutics—are frequently ineffective in the long term. Glioblastomas possess a remarkable resistance to these modalities, largely due to their ability to suppress immune responses and the formidable barrier of the blood-brain interface, which limits the accessibility of most pharmacological agents to the brain. Following surgical intervention, recurrence is nearly universal, resulting in the further spread of the tumor and heightened challenges for patient care.
In light of these daunting challenges, immunotherapy has emerged as a beacon of hope in glioblastoma research. This innovative strategy seeks to harness the body’s immune system to specifically target and eradicate cancer cells. The field of immunotherapy is rapidly evolving, showing potential applications not just in oncology but also in treating autoimmune disorders, chronic infections, and even allergies. Unlike conventional treatments, immunotherapy could offer a more dynamic approach to managing cancers, including glioblastoma.
However, researchers encounter several hurdles when applying immunotherapy to glioblastoma. The tumor’s evolving nature ensures it presents a multitude of mutations across different brain regions, complicating the targeting process. Nonetheless, preliminary clinical trials have indicated avenues of promise; for instance, the administration of immunotherapies through injections into the cerebrospinal fluid has demonstrated safety, prompting scholars to refine these methodologies for improved effectiveness.
Despite the promise that immunotherapy holds, turning this hope into reality is not without its complications. Funding shortages have historically limited brain cancer research, although new initiatives are emerging to attract experts from various scientific fields. I bring two decades of experience studying immune system manipulation in cancer settings and chronic infections; my recent focus has shifted to investigating how immune cells can influence cerebral functions, paving the way for interventions that circumvent barriers limiting treatment reach to glioblastoma tumors.
As part of a global coalition aiming to generate and evaluate immunotherapeutic options specifically targeted toward glioblastoma, my pursuits are underscored by a dedication to improving patient outcomes. While the complexities surrounding glioblastoma treatment are daunting, the exploration of immunotherapy represents a critical opportunity to enhance care and potentially prolong survival.
While the future of immunotherapy for glioblastoma projects excitement, navigating the landscape of treatment options requires considerable caution. Not all cancers respond uniformly to immunotherapeutic approaches, and patients may face immune-related adverse effects, such as organ inflammation and brain swelling. The method of delivery is also critical—non-invasive avenues, such as intravenous injections or spinal administration, provide a significant advantage over more invasive cranial surgeries.
As interest and investment in glioblastoma immunotherapy grow, the research community remains optimistic. Although therapeutic avenues for glioblastoma still pose significant obstacles, dedicated efforts could soon lead to breakthroughs that might dramatically improve the lives of those battling this formidable and heartbreaking disease.