Herpes simplex virus type 1 (HSV-1), widely recognized for causing cold sores, has recently been spotlighted in scientific research for its potential implications in neurodegenerative diseases. A recent study conducted by researchers from the University of Colorado and the University of Bourgogne has illuminated the ways in which HSV-1 interacts with the brain, mapping its effects on various neural regions. This exploration not only enhances our understanding of the virus itself but also opens avenues for investigating its role in conditions like Alzheimer’s disease.
Understanding how HSV-1 infiltrates the central nervous system (CNS) is crucial for grasping its broader neurological effects. The study presented two main pathways: the trigeminal nerve and the olfactory nerve. While these entry points have been established, the progression of the virus through the brain remains less defined. Neurologist Christy Niemeyer emphasized that the lack of understanding regarding the pathways of CNS invasion and the specific brain regions vulnerable to infection hampers efforts to fully comprehend how HSV-1 might initiate neurodegenerative disease processes.
This knowledge gap is significant given the virus’s association with neurodegenerative conditions, particularly Alzheimer’s disease. Prior to this study, researchers suspected a connection but lacked definitive insights into the mechanics of HSV-1’s neurological invasion. Thus, classifying these pathways and their implications is a foundation for future research.
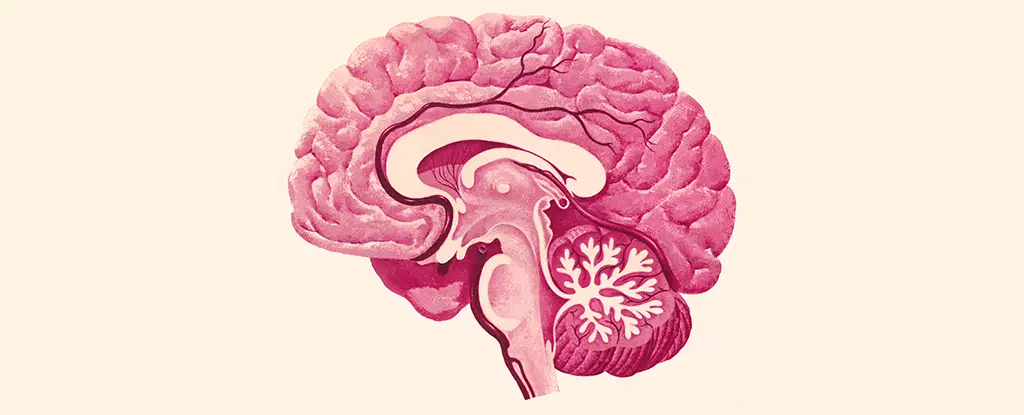
The researchers delved into the specific brain areas affected by HSV-1. Notably, they discovered substantial viral presence in critical regions such as the brainstem and hypothalamus. The brainstem is integral for autonomic functions such as heart rate, respiration, and movement control, while the hypothalamus regulates homeostatic functions like appetite and hormonal balance. Conversely, regions notably related to memory and spatial navigation—the hippocampus and cortex—remained largely unscathed by the viral antigens.
This finding raises important questions about the selective vulnerability of certain brain regions. It suggests that while HSV-1 can influence fundamental bodily functions through its presence in the brainstem and hypothalamus, it doesn’t directly impair memory-related functions, at least not through the same initial viral invasion. Understanding why certain areas are affected while others are spared could provide vital clues about neuroprotection and resilience in the face of viral infection.
The study further analyzed the response of microglia, the resident immune cells of the CNS, to HSV-1 infiltration. In response to viral presence, microglia exhibited inflammation in the affected brain regions, which persisted long after the virus was cleared. This could indicate ongoing damage or dysfunction within these regions, even without a full-blown encephalitis episode.
Chronic inflammation is increasingly being associated with various neurological disorders, including Alzheimer’s disease. As Niemeyer pointed out, the implications of persistently inflamed microglia could extend beyond the immediate effects of HSV-1. The news that immune activation can linger after the initial infection presents a potential mechanism through which HSV-1 might exacerbate or even trigger neurodegenerative processes later in life.
The intersection of HSV-1 infection and neurodegenerative conditions, especially Alzheimer’s, is a burgeoning area of interest. The study highlights the necessity for further investigation into how viral infections contribute to cognitive decline and degeneration. There’s a compelling case that HSV-1’s interaction with microglia could play a making role in the chronic inflammatory state that is a hallmark of neurodegeneration.
With the groundwork laid by this research, future studies may be able to explore therapeutic avenues that target both the viral aspects and the inflammatory responses to mitigate the potential risks associated with HSV-1. It opens a new paradigm in understanding Alzheimer’s and other neurodegenerative diseases—one in which viral infection and chronic inflammation may synergistically contribute to cognitive decline.
This groundbreaking study sheds light on the complex relationship between HSV-1 and brain health. By elucidating the virus’s entry routes, the specific brain regions it affects, and the role inflammation plays, it paves the way for novel therapeutic strategies and a deeper appreciation of the interconnectedness of viral and neurological health.