In a world suddenly gripped by a pandemic, the importance of understanding infectious diseases has leaped from academic discussions into everyday consciousness. The film *Contagion*, which once seemed a speculative thriller, now resonates with disturbing realism. Its detailed portrayal of how viruses can stealthily infiltrate populations serves as a stark reminder of how fragile our defenses really are. At the core of this understanding is a seemingly simple but profoundly impactful metric: R0, or the basic reproduction number.
R0 functions as the compass guiding us through the labyrinth of infectious diseases. It encapsulates how easily a pathogen can spread in a fully susceptible population. When R0 exceeds one, the infection accelerates exponentially, turning a single case into a raging outbreak. An R0 below one signifies that the disease is likely to fade away over time. This numerical representation isn’t just an academic statistic; it’s a reflection of how our environments, behaviors, and interventions influence the trajectory of a disease.
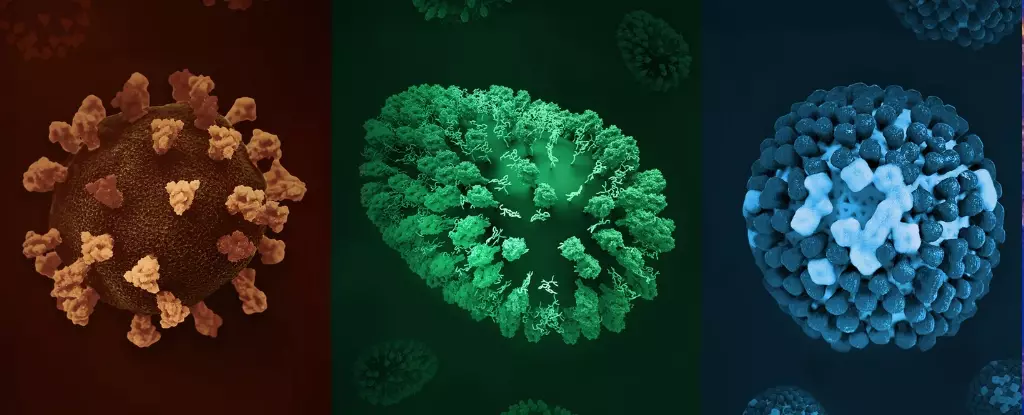
What makes the concept of R0 so compelling is its accessibility and its capacity to predict. It’s not a static figure but a dynamic measure heavily influenced by countless factors including pathogen biology, human behavior, and societal structure. For example, highly infectious diseases like measles boast R0 values between 12 and 18, meaning one person can ignite a chain of infections affecting hundreds. Conversely, diseases like leprosy or MERS have R0s below one, indicating a much slower or less efficient transmission, yet they still pose grave health threats. This disparity highlights that a lower R0 does not equate to safety—especially when healthcare systems are overwhelmed or when the pathogen causes severe illness.
Reassessing Risk: The Reality of Highly Contagious Diseases
Among the spectrum of infectious diseases, measles emerges as a formidable foe. Its extraordinarily high R0 indicates its viral particles are incredibly infectious—airborne droplets containing tiny infectious particles linger in the environment for hours. This means an unvaccinated person entering a contaminated space can contract measles long after the initially infected individual leaves. Such contagiousness exposes glaring vulnerabilities in public health infrastructure—gaps in vaccination rates elevate the risk of outbreaks. Recent trends, accentuated by the COVID pandemic’s disruption and misinformation campaigns, have caused immunization rates to decline, reviving measles outbreaks even in developed countries.
COVID-19, with R0 estimates generally between eight and twelve depending on the variant, underscores how even less contagious viruses can cause global upheaval. Despite advancements, the virus’s ability to spread via aerosols and the fact that asymptomatic individuals can unknowingly transmit it complicate containment efforts. This emphasizes a crucial lesson: pathogen transmissibility is a core determinant—not the sole one, but a crucial one—in shaping public health strategies.
On the other end of the contagiousness spectrum, diseases like tuberculosis demonstrate that lower R0 values do not equate to benignity. TB’s R0, often below one in some regions but up to four in crowded, impoverished settings, highlights how socio-economic factors dramatically influence disease spread. TB’s slow progression and the requirement of prolonged contact make it insidious, especially considering the increasing prevalence of drug-resistant strains that complicate treatment and containment efforts.
Less Noticeable but Equally Dangerous Threats
While the world fixates on highly infectious diseases, lesser contagions like Ebola’s R0 (around 1.5 to 2.5) hide in plain sight. Ebola’s transmission necessitates close physical contact, typically during caregiving or funerals, making its spread less random but devastating when it occurs. Its high fatality rate and ability to cause hemorrhagic fever mean even limited transmission can be catastrophic.
Leprosy and MERS, with R0s below one, exemplify how diseases can remain dormant or confined within specific contexts without causing widespread outbreaks. Yet, their severity—such as the lifelong disabilities associated with leprosy—reminds us that low transmissibility does not imply low impact. Risk is a multifaceted equation, combining infectivity with disease severity, treatment options, and societal vulnerabilities.
A critical realization emerges: the key to controlling infectious diseases lies not only in individual precautions but also in collective immunity and public health infrastructure. Vaccinations drastically reduce R0 by lowering susceptibility, transforming potentially explosive outbreaks into contained incidents. Herd immunity acts as an invisible barrier, protecting even those who cannot be vaccinated. By understanding how diseases spread—through droplets, fomites, vectors, or bodily fluids—we can tailor intervention strategies that maximize effectiveness.
The Power of Knowledge: Protecting Society as a Whole
In our interconnected world, dissecting the mechanics of disease transmission gives us strategic advantage. Recognizing the roles of fomites—objects like doorknobs, elevator buttons, and water fountains—reminds us that infection control extends beyond personal hygiene. Disinfecting surfaces and practicing social distancing are not mere inconveniences but vital defenses rooted in science.
This knowledge empowers us to challenge misinformation, which often inflates fears or underestimates threats. It helps us understand why vaccines are critical, not just personal protection but as a societal duty. When vaccination coverage drops, the R0 for highly contagious diseases like measles surges, leading to outbreaks that threaten vulnerable populations.
As the global health landscape continues to evolve, the lessons embedded in the concept of R0 are more relevant than ever. They emphasize that infectious diseases are not just biological phenomena but social challenges that require coordinated action, sound policies, and informed communities. Recognizing the nuanced interplay between pathogen characteristics and societal factors can tip the balance in favor of health, resilience, and ultimately, survival.