Breast cancer remains one of the most formidable adversaries in modern medicine, with nearly 30% of successful treatments thwarted by tumor recurrence. Despite remarkable advances in early detection and targeted therapies, the haunting possibility of cancer returning casts a long shadow over survivors’ lives. It’s not just a matter of physical health but psychological well-being, as the dread of relapse influences long-term quality of life. This persistent threat underscores an urgent need for innovative strategies that go beyond conventional monitoring. Instead of merely waiting for signs of relapse, the scientific community is carving a new path—aiming to eliminate the root causes of recurrence: dormant tumor cells.
Unmasking the Dormant Tumor Cell Threat
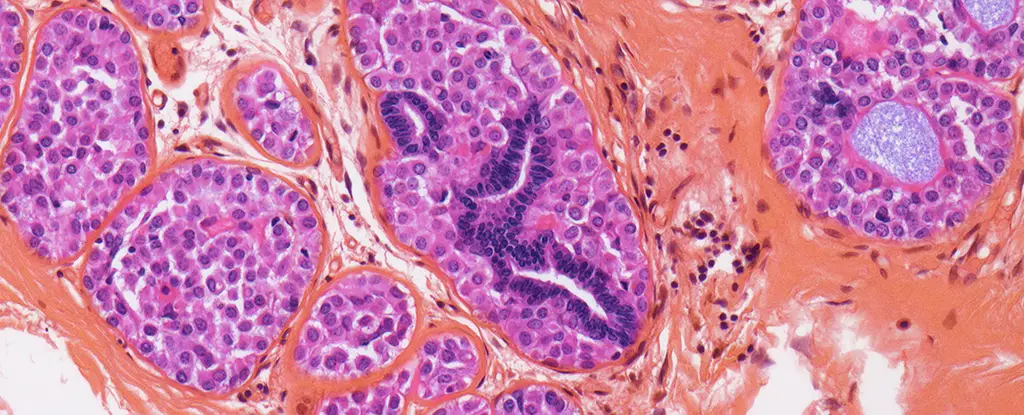
For decades, the concept of ‘cancer dormancy’ remained an elusive puzzle. These cells, often lying inactive in the bone marrow and other tissues, pose a treacherous threat—they are invisible to immune surveillance and resilient to many treatments. Recently, however, researchers have confirmed that DTCs (dormant tumor cells) are crucial in understanding why some cancers reappear years, even decades, after initial remission. The core challenge was identifying how to target this covert population without harming healthy tissue. The breakthrough came when scientists demonstrated that specific drugs could selectively attack these ‘sleeping’ cells, preventing them from awakening to reignite the disease.
Transformative Research: Targeting the Roots, Not Just the Symptoms
A pioneering study led by scientists at the University of Pennsylvania marks a monumental shift in the fight against breast cancer recurrence. The researchers adopted a proactive approach—focusing on eradicating DTCs rather than waiting for their resurgence. By harnessing the power of existing medications like hydroxychloroquine, traditionally used for autoimmune disorders, and everolimus, an established anti-cancer drug, the team achieved astonishing results. In trials involving 51 patients with confirmed dormant tumor cells, combining these drugs eradicated up to 87% of DTCs. The implications are profound: a potential paradigm shift from reactive treatment to preemptive eradication.
What makes this approach particularly promising is not just the high clearance rate but also the stark reality that all participants who received both drugs remained completely cancer-free after three years. Even those on single medications experienced survival rates exceeding 90%. These findings suggest that targeting dormant cells could take a significant bite out of the mortality caused by breast cancer, fundamentally changing prognosis and survival statistics.
Understanding the Mechanisms and Broader Implications
The success of these dual-drug therapies led researchers to delve into the biological underpinnings of dormant tumor cells. They uncovered that these cells respond differently to treatments than their actively dividing counterparts. While traditional chemotherapies target rapidly proliferating cells, DTCs exhibit unique survival mechanisms that render many drugs ineffective. The drugs used in the study seem to interfere with these survival pathways, effectively rendering the dormant cells vulnerable.
This revelation is a wake-up call for oncology: the biology of dormancy is distinct and requires tailored strategies. More importantly, the findings illuminate a broader principle—that drugs ineffective against active tumors might still be potent against dormant populations if we understand and exploit their unique biology. The potential for existing medications to be repurposed in this way accelerates the pathway to clinical application, bypassing the lengthy development of entirely new drugs.
Looking Towards a Future of Preventive Oncology
While these findings spark hope, caution remains essential. Not all breast cancer survivors harbor dormant tumor cells, and identifying those at risk will be a vital step in personalizing treatment plans. Future research must focus on refining drug combinations, doses, and treatment durations to maximize efficacy and minimize side effects.
What stands out most in this emerging landscape is the possibility that we can shift from a model of crisis management to one of prevention. Instead of dealing with relapses after they scrape through the immune system, scientists aim to eliminate the very seeds of future recurrence. This strategy not only promises longer, healthier lives for survivors but also reduces the emotional toll associated with the fear of relapse. As this research advances, it might redefine how we approach not just breast cancer, but potentially other cancers riddled with dormant cell populations, ushering in an era where the hope of truly lasting remission becomes a tangible reality.