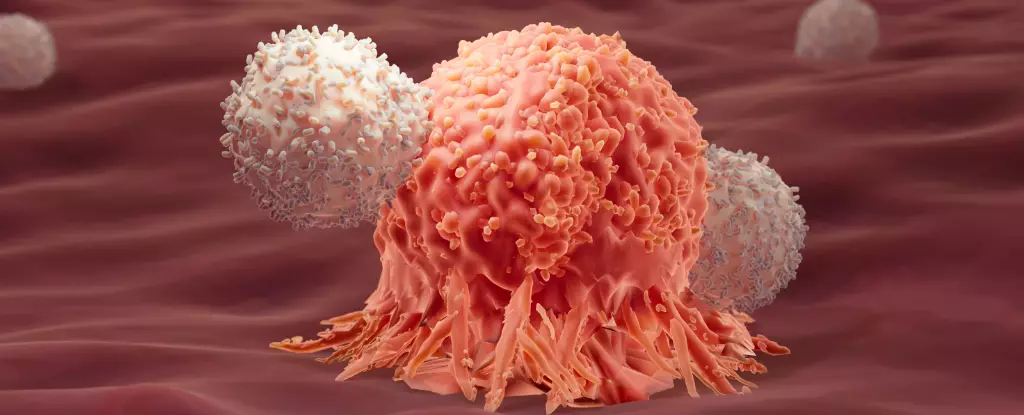
Recent research has opened up intriguing possibilities for enhancing cancer treatment through a deeper understanding of the immune system’s responses. Traditional immunotherapy has been a beacon of hope, utilizing a patient’s own immune defenses to engage in a war against cancerous cells. However, this battlefield is more complex than it seems. While immunotherapy has led to remarkable successes, the inconsistency in outcomes raises fundamental questions: what makes some patients respond favorably to these treatments while others succumb to relapse?
Scientists have dedicated themselves to unraveling these complexities. Their latest investigations have unveiled an unexpected synergy between two different immune responses—previously deemed contradictory. This duality, described metaphorically as “yin and yang,” may hold the key to augmenting the efficacy of current cancer therapies. A series of studies illustrate how manipulating different facets of the immune response can lead to potentially life-saving outcomes.
A pivotal study led by researchers at EPFL explored why certain patients exhibited long-term remission from acute lymphoblastic leukemia (ALL) after undergoing CAR-T cell therapy, a cutting-edge form of immunotherapy. The team meticulously analyzed genetic information derived from nearly 700,000 CAR-T cells across 82 patients to construct a comprehensive genetic map.
Intriguingly, the findings indicated that patients who enjoyed prolonged remission had immune profiles that suggested a unique combination of immune responses, particularly a juxtaposition of type 1 (which traditionally targets cancer cells) and type 2 responses, which are typically involved in combating larger parasites. This odd link insinuates that type 2 responses—often dismissed as non-essential or even detrimental in the context of cancer—may actually provide supportive mechanisms that bolster therapeutic efficacy.
Building upon these revelations, a follow-up study involving mouse models deepened the inquiry by comparing the effects of single versus dual immune responses in the context of cancer treatment. The experimental design featured one cohort receiving a conventional approach utilizing type 1 immune responses alone, while another group received a dual treatment, integrating both type 1 and modified type 2 proteins. The outcomes were striking: 86% of the mice that received the combined treatment exhibited full remission, showcasing the profound impact that an integrated immune strategy can wield against malignancies.
Moreover, the cured mice demonstrated remarkable resilience when exposed to new tumors weeks later, suggesting that the modified immune proteins potentially enhanced the T cells’ stamina and energy through a metabolic boost via glycolysis. This phenomenon could signify a pioneering edge in developing therapies that not only initiate a tumor attack but also sustain long-term immune vigilance against recurrences.
The implications of these findings stretch beyond mere academic interest; they herald a potential revolution in how we approach cancer immunotherapy. Traditionally, immunotherapies have concentrated solely on type 1 immune responses, leading to an oversight of the possible benefits that a comprehensive approach could provide. Understanding this synergy could catalyze the development of more refined and successful immunotherapeutic strategies that bridge the gap between efficacy and survivorship.
Researchers advocate for further exploration into the mechanisms underlying type 2 immune responses. While correlations between type 2 factors and long-term remission have been identified, it’s critical to discern causative pathways that might explain these associations. Additionally, a stout emphasis on continued trials and clinical studies is essential to validate these early findings and optimize treatment protocols for human applications.
Moving Forward: A New Paradigm in Cancer Therapy
As the narrative around cancer therapy evolves, it is evident that the immune system embodies remarkable potential that has yet to be fully realized. The interplay between diverse immune responses—as demonstrated through the innovative research exploring “yin and yang” immunity—could reshape the landscape of oncological treatments.
Ultimately, the goal is to translate these scientific discoveries into clinical realities, crafting personalized therapies that not only combat tumor growth but also fortify the immune system’s resilience against future threats. The newfound understanding of the immune responses could pave the way for advanced immunotherapies that bring us closer to a future where long-term remission becomes a standard rather than an exception in cancer management.