For decades, neuroscience has confined glycogen primarily to the realm of muscle and liver function, viewing it as a transient energy reservoir that supports physical activity and metabolic stability. However, recent groundbreaking research turns this assumption on its head, suggesting that glycogen stored within neural tissue may be far more influential in brain health—and disease—than previously acknowledged. If we accept this paradigm shift, the implications for understanding neurodegenerative conditions like Alzheimer’s disease could be revolutionary, opening potential pathways for innovative therapies that target the brain’s own metabolic machinery.
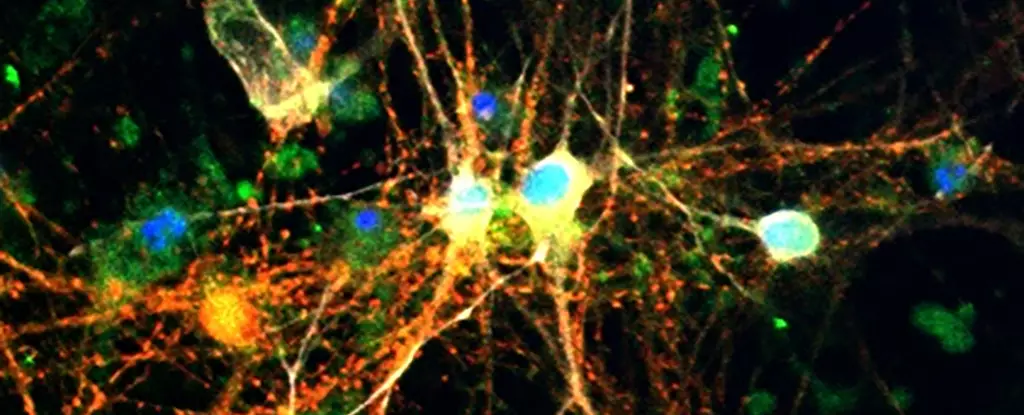
The new evidence indicates that glycogen in the brain isn’t just a passive energy store; instead, it actively participates in the complex pathogenesis of neurodegeneration. This insight, emerging from the Buck Institute for Research on Aging, positions glycogen as a critical player in neuronal health, particularly in conditions characterized by abnormal protein accumulation such as tauopathies. It suggests that discrepancies in glycogen metabolism—traditionally associated with muscle and hepatic function—are deeply intertwined with the deterioration seen in Alzheimer’s and similar diseases. This revelation forces us to reconsider the nuanced role of energy regulation within the neural environment, emphasizing that what was once considered a simple backup system may actually be central to the cell’s fate.
Linking Glycogen Dysregulation to Tauopathies
A core discovery from this research spotlighted excessive glycogen levels in models of tauopathy and in human Alzheimer’s brains. Inside neurons, toxicity appears to be compounded by the buildup of both tau proteins and glycogen, creating a damaging feedback loop. Crucially, this isn’t merely an incidental co-occurrence but seems to reflect a direct interference of tau with glycogen metabolism. The tau proteins disrupt normal enzymatic activity responsible for breaking down glycogen, notably through impairing glycogen phosphorylase, or GlyP—a key enzyme tasked with liberating energy from stored glycogen.
This mechanistic insight is particularly compelling because it highlights a specific point of intervention: restoring or enhancing GlyP activity. Experimental increases of GlyP in fruit fly models yielded promising results, reducing glycogen accumulation, diminishing cellular damage, and extending lifespan. This demonstrates that bolstering the brain’s capacity to effectively manage glycogen could fundamentally alter disease progression. It challenges the notion of neurodegeneration as merely a consequence of protein misfolding, positioning metabolic dysregulation as an active driver—perhaps even a trigger—in the pathological cascade.
Dietary and Pharmacological Interventions as Therapeutic Strategies
One of the most intriguing facets of this research lies in the potential for accessible intervention strategies. The study reveals that dietary modifications—specifically, low-protein diets—can mimic the beneficial effects of increased GlyP activity, resulting in reduced brain damage and improved survival in tauopathy models. Such findings link metabolic flexibility to neural resilience and suggest that simple lifestyle changes could have profound impacts on neurodegenerative trajectories.
Building on this, the team developed a drug based on 8-Br-cAMP, which simulates the molecular effects of dietary restriction. The drug’s ability to restore glycogen metabolism in experimental models signals a promising avenue for pharmaceutical development. Furthermore, existing medications targeting metabolic pathways, notably GLP-1 receptor agonists like Ozempic, are emerging as potential neuroprotective agents. These drugs, primarily designed for diabetes management, might inadvertently modulate glycogen pathways indirectly, offering hope that repurposing could expedite the development of effective treatments for cognitive decline.
The overarching implication is that effective management of brain glycogen could serve as a pivotal node in combating neurodegeneration. If metabolic health influences tau aggregation and neuronal survival, then therapies which optimize glycogen processing could slow or even reverse the course of diseases like Alzheimer’s. This paradigm reimagines the approach to neurodegenerative diseases—not solely focusing on clearing protein aggregates but also targeting the fundamental metabolic disturbances that facilitate their formation.
The Future of Brain Disease Treatment Lies in Metabolic Mastery
By illuminating glycogen’s underestimated role within the nervous system, this research paves the way for a new therapeutic frontier. It underscores the importance of metabolic regulation—how neurons manage, store, and utilize energy—as central to maintaining cognitive health. This perspective encourages a broader, more integrative approach to neurodegenerative disease management, one that encompasses diet, pharmacology, and the modulation of intracellular metabolic pathways.
The prospect of shifting clinical focus towards enhancing glycogen metabolism warrants a reassessment of current therapeutic strategies. It suggests that rather than solely targeting pathological proteins like tau, addressing the underlying metabolic dysfunction might yield more sustainable and impactful results. In essence, fixing the brain’s energy balance could prevent or mitigate the molecular chaos that leads to neuronal death. As research progresses, it becomes increasingly clear that unlocking glycogen’s full potential inside the brain might be the key to combating aging-related cognitive decline—transforming hope into achievable reality.