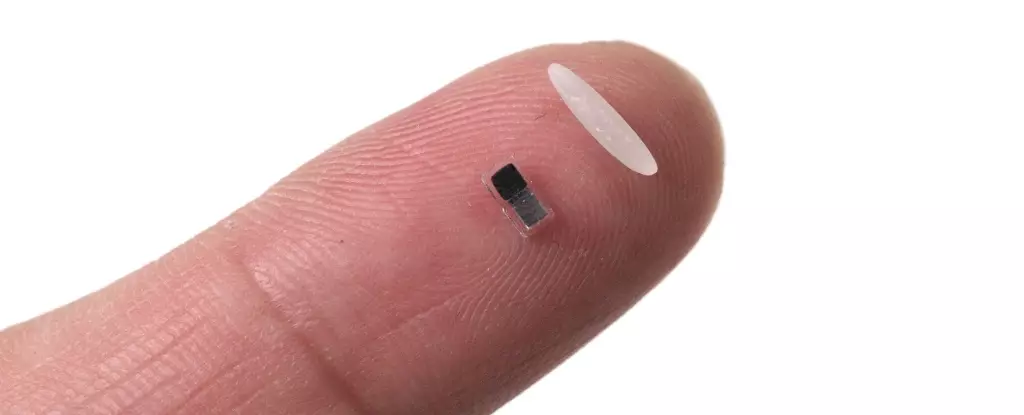
A remarkable innovation in cardiac care has captured the attention of the medical community: the world’s smallest pacemaker, an extraordinary device that holds the potential to reshape how we approach heart health. Smaller than a grain of rice, this intriguing device can be injected into the body, controlled by light, and safely dissolve once its job is complete. Although clinical testing on humans is still a few years away, this technological leap has been described as a game-changing development that could influence various medical fields.
The motivation driving this innovation is heart-wrenching yet compelling: it aims to assist the approximately one percent of children born worldwide with congenital heart defects, who often require a temporary pacemaker in the immediate aftermath of surgery. Currently, the existing methods involve invasive procedures that can pose additional risks. With the new pacemaker, patients may breathe easier, knowing they have a reliable, non-invasive option at their disposal during crucial recovery periods.
From Surgical Dependency to Wireless Freedom
Traditional temporary pacemakers present various complications, from the invasive surgery required to connect electrodes to the heart muscle to the concerns surrounding the removal process. Notably, serious incidents can occur during this removal, as evidenced by the tragic fate of Neil Armstrong, who suffered fatal internal bleeding due to complications following pacemaker extraction. This grim precedent highlights a vital need for less invasive approaches in cardiac care.
The revolutionary feature of the new pacemaker is its wireless design, which eliminates the need for cumbersome wires and external devices typically strapped to the patient’s chest. The pacemaker is paired with a soft patch that adheres to the chest and uses light signals to guide its functioning. Specifically, when the patch senses irregularities in the heartbeat, it emits light that instructs the pacemaker to deliver appropriate electrical pulses, restoring rhythm in a way that is highly responsive and precise.
How the Technology Works
Delving deeper into the mechanics behind this groundbreaking device reveals its ingenuity: the pacemaker is powered by a galvanic cell — a system harnessing the body’s own fluids to convert chemical energy into electrical energy. This innovative approach allows for a seamless integration of the device into the patient’s physiology, further minimizing disruption to normal bodily functions.
The device’s efficacy has been tested across various animal models, including mice, rats, pigs, and dogs, alongside human heart tissues in laboratory settings. John Rogers, a senior author on the study and a principal researcher at Northwestern University, expresses optimism that human trials could commence in a two to three-year timeframe. This development is promising, not just for patients needing temporary pacemakers, but for advancing our understanding and treatment of heart conditions at large.
Potential Implications Beyond Cardiovascular Health
What’s particularly hopeful is the thought that the underlying technology behind this tiny pacemaker could extend far beyond the realm of cardiology. Experts like Bozhi Tian of the University of Chicago have noted that this device marks a significant advancement in bioelectronic medicine, suggesting its principles could tackle other challenges such as nerve regeneration and wound healing. As the medical world grapples with the ever-increasing burden of chronic disease, innovations like this present a potent opportunity to streamline care while enhancing patient outcomes.
The impact of heart disease, dubbed the leading cause of mortality globally, cannot be overstated. Hence, the success of this miniature pacemaker could herald a new dawn in both prevention and treatment strategies.
The advent of this tiny pacemaker is not merely an intriguing technical achievement; it symbolizes a larger movement towards more intelligent, adaptable, and patient-centered healthcare solutions. While still in the developmental phase, the excitement surrounding its future application underscores a profound opportunity for reimagining the landscape of medical advances in cardiology and beyond.