The quest for understanding and remedying the critical impacts of sudden cardiac arrest (SCA) on brain functionality has reached a notable milestone. Recent research conducted by a team in China involves a groundbreaking experiment where brain activity in pigs was revived nearly an hour after circulation ceased. This advancement not only holds promise for enhancing resuscitation protocols but also provides significant insights into the interplay between different organs during recovery after cardiac arrest.
Sudden cardiac arrest is a medical emergency marked by the abrupt termination of blood flow caused by the heart’s failure to pump effectively. This leads to ischemia, which can have dire consequences, particularly on the brain. Research shows that the brain is vulnerable to damage shortly after blood flow is interrupted, with significant neuronal injury occurring within mere minutes. Consequently, the effective window for resuscitation is alarmingly brief. Moreover, ischemia does not solely affect the brain; it hampers multiple organs, complicating recovery efforts and outcomes.
While previous studies have highlighted the effects of multi-organ ischemia on brain recovery, the specific contributions of individual organs have largely gone unexplored. This gap in research sparked innovation among scientists, leading them to investigate the potential role of the liver, an organ critical for blood purification and metabolic processes, in facilitating brain recovery. Traditionally underappreciated in this context, the liver’s involvement during periods of ischemia has now come to the forefront of scientific inquiry.
An Innovative Experimental Approach
In a pivotal study led by physician Xiaoshun He from Sun Yat-Sen University, a cohort of 17 lab-raised Tibetan minipigs was utilized. The researchers designed a series of experiments to discern the effects of liver involvement during instances of brain ischemia. Two groups of pigs faced consecutive ischemic episodes centered around a controlled 30-minute blood deprivation. One group was also subjected to liver ischemia, while the other was not. A control group was introduced, which underwent no ischemic conditions. Notably, when the pigs were euthanized for analysis, the control group exhibited minimal brain damage, while that of the liver-ischemic group showed significantly more damage compared to their non-liver-ischemic counterparts.
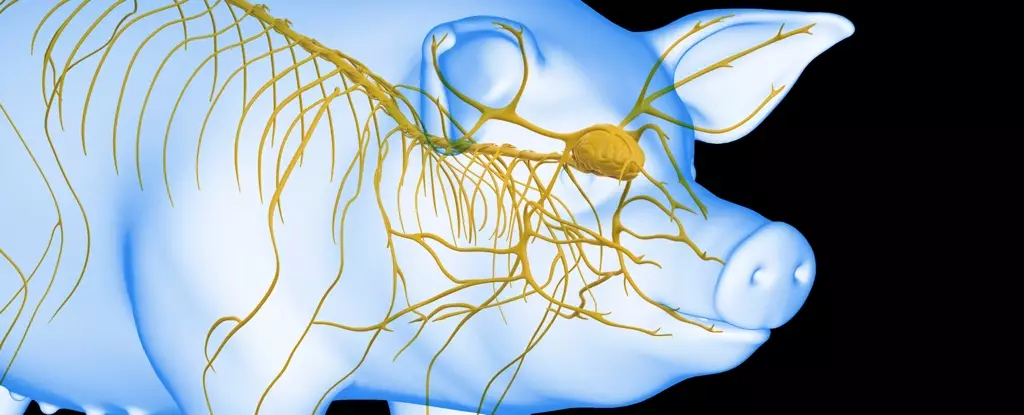
The next logical progression in this research aimed to connect an undamaged liver to the life support systems utilized during brain resuscitation. Although this procedure is far from a practical application in humans, its exploratory nature unveils critical insights regarding the optimal timeframe for initiating resuscitation. In these experimental setups, an artificial heart and lungs facilitated fluid circulation to the brain, while a pig’s liver was incorporated as a critical support entity, termed liver-assisted brain normothermic machine perfusion.
The experimental timeline was vital. When brains were connected to the artificial life support 10 minutes post-initiation of the system, a notable but brief return of electrical activity was recorded within half an hour. Variations in connection intervals produced even more compelling results, particularly at the critical 50-minute mark. Here, brains deprived of oxygen resumed electrical function and maintained it for an impressive six hours. Conversely, after 60 minutes of blood deprivation, activity only resurfaced for three hours, illustrating a stringent time frame where the therapeutic benefits of an intact liver had the most pronounced effects.
The findings from this innovative study reveal more than just the mechanics of lost and restored brain activity. They invite a re-evaluation of resuscitation protocols and stress the necessity of considering organ interactions in recovery protocols following cardiac events. By underscoring the liver’s significant contribution to brain recovery post-cardiac arrest, this research opens new pathways for exploring treatment options and enhancing patient survival rates.
The prospect of improving outcomes for individuals experiencing cardiac arrest remains a pressing medical challenge. Moving forward, further investigations into organ interplay and their respective roles during ischemic conditions will be paramount. Ultimately, should these insights translate into clinical practice, they could revolutionize the management of cardiac arrest cases and reshape our understanding of organ collaboration in the face of critical emergencies.