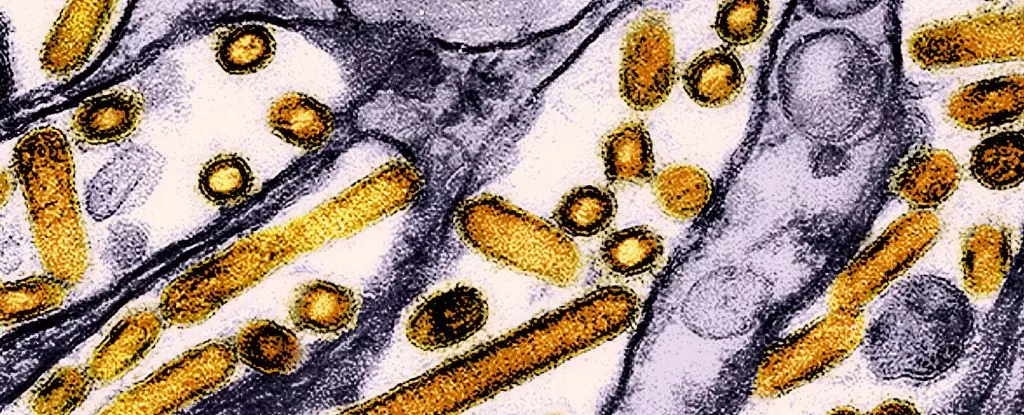
The emergence of cases of highly pathogenic avian influenza (H5N1) among humans, particularly among dairy workers in the United States, has prompted a fresh wave of anxiety concerning zoonotic diseases. A recent study examining blood samples from 115 dairy workers in Michigan and Colorado found that approximately 7 percent exhibited antibodies for the virulent strain of H5N1. While this discovery has underscored that a significant number of individuals may face mild or asymptomatic infections, it also raises alarm bells about the potential for the virus to become a more serious public health threat.
Between June and August 2024, researchers from the U.S. Centers for Disease Control and Prevention (CDC) conducted tests which revealed that many workers who came into contact with potentially infected cattle were unaware of their exposure. Notably, half of those who showed signs of prior infection reported no severe symptoms. This indicates that while some individuals may have contracted the virus without serious consequence, the insidious nature of H5N1 could allow it to spread unchecked, enhancing its capacity for mutation into more virulent forms.
This analysis emphasizes a broader issue—the potential for pathogens to evolve, particularly in a climate where neglecting preventative measures is commonplace. The current circumstances present a crucial opportunity to address the gap between existing biosecurity measures and real-world practices among agricultural workers.
Recent events in Cambodia serve as a potent reminder of how rapidly the nature of a virus can change. Reports indicate that a hybrid strain of bird flu has caused fatalities among human patients, underscoring the pathogen’s capacity for mutation and increased virulence. Early studies suggest that this strain might facilitate airborne transmission and effectively infect mammals, raising concerns for global public health.
Moreover, the emergence of a similar strain in Canada, which has critically affected a teenager who contracted the virus from infected dairy cows, further illustrates the gravity of the situation. The potential for human-to-human transmission, indicated by the genetic changes observed, underscores why experts are advocating for heightened surveillance and stringent control measures.
The findings from the CDC report stress an alarming trend: many dairy workers are not utilizing the recommended personal protective equipment (PPE) while engaging with infected animals. As highlighted in the report authored by CDC health scientist Alexandra Mellis, this negligence raises serious questions about the adequacy of training and resources available to these workers.
The demographic of these workers adds another layer to this concern, as many of them belong to Spanish-speaking communities who may have distinct cultural needs that should be met through tailored outreach efforts. Efforts to improve communication and training regarding safety measures are not only vital but imperative to minimize future disease transmission.
The alarming reality is that, as of now, over 400 dairy herds across 48 U.S. states have been infected with the highly pathogenic avian influenza. The mass culling of domestic birds, surpassing 90 million since 2022, highlights the severe impact this disease has had on both public health and agricultural sectors. As authorities shift their focus to vaccination programs for endangered species like California condors, it becomes increasingly clear that a multi-faceted approach is necessary.
This encompasses not only veterinary medicine and wildlife protection but also a proactive stance on human health. The urgency to develop a human vaccine against bird flu must be recognized by researchers, health professionals, and policymakers alike. The combined efforts of these stakeholders are crucial in mitigating risks and preventing future outbreaks.
The detection of H5N1 antibodies among dairy workers poses a significant public health concern that cannot be overlooked. The reported mild symptoms should not be a cause for complacency, as they could be indicative of broader, unchecked viral spread leading to more severe strains. The cross-border implications of outbreaks, as demonstrated in Cambodia and Canada, reinforce the necessity for continuous monitoring and intervention strategies.
Moving forward, it is imperative that we collectively embrace a culture of vigilance and preparedness. Crucially, this entails better education for workers in agriculture, improved biosecurity protocols, and a commitment to scientific research aimed at both vaccination and effective public health responses. By addressing the risks and challenges associated with the spread of bird flu, we can safeguard both our health and the health of future generations.