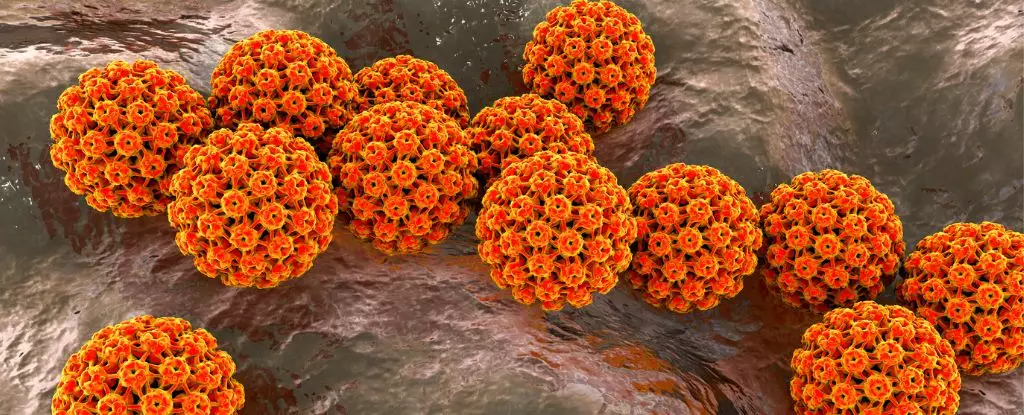
Recent studies have thrown a spotlight on the risks men face regarding oral human papillomavirus (HPV), particularly the strains associated with various cancers. Oral HPV has often been overlooked compared to its counterpart in cervical cancer, mainly because much of the research has historically centered around women and their health issues. However, the findings indicate that men, irrespective of their age, are at considerable risk of contracting HPV-associated cancers affecting the mouth and throat. This raises urgent questions around public health strategies aimed at preventing such infections, especially concerning vaccination policies that fall short for men who could greatly benefit from them.
Oropharyngeal cancers, which once were relatively rare, are now emergently prevalent, especially in regions like the United States and parts of Europe. Alarmingly, men are diagnosed with these cancers at rates significantly higher than women, with this trend persisting even among those who lack traditional risk factors such as smoking or excessive alcohol consumption. Research conducted across diverse populations in the U.S., Brazil, and Mexico underscores the connection between new instances of HPV and the rising cancer rates.
The study, which involved a substantial cohort of healthy men aged 18 to 70, compellingly demonstrated that the acquisition risk of cancer-associated HPV strains does not diminish with age. This contradicts the longstanding belief that vaccination efforts should mainly target younger males. Instead, the data presents a clear message: susceptibility to HPV infection remains consistent throughout adulthood, thereby emphasizing the need for wider vaccination coverage that includes middle-aged men who might have missed out on the opportunity earlier in life.
The introduction of the HPV vaccine is a significant advancement in cancer prevention, offering protection against high-risk strains such as HPV-16 and HPV-18, which are notorious for their role in oral cancers. Despite this, vaccination rates among young males remain disproportionately lower compared to females. This imbalance contributes to the worrying uptick in oropharyngeal cancer rates, even as cervical cancer cases decrease dramatically due to successful vaccination campaigns.
Current recommendations from the Centers for Disease Control and Prevention (CDC) endorse HPV vaccinations for young individuals up to the age of 26. However, the limitations that exist beyond this age—where the vaccine is primarily offered to immunocompromised individuals or those with specific risk factors—must be critically examined. The CDC notes, “HPV vaccination of people in this age range provides less benefit,” yet the evidence suggests that there may still be significant advantages for many men even in their 30s and beyond.
Throughout the years, most HPV research has focused primarily on men who engage in sexual activities with other men, leaving a gap in understanding how the virus impacts heterosexual men. The transmission methods are not limited to sexual intercourse; HPV can also spread through skin contact, fingers, and even shared drinking utensils. This complexity means that developing a comprehensive understanding of HPV transmission is crucial for establishing effective public health campaigns.
The recent study conducted by researchers at the renowned Moffitt Cancer Center reinforces the urgent need for continued vigilance against oral HPV infections. Nearly 20% of the cohort tested positive for an existing oral HPV strain, with approximately 6% carrying a cancer-causing variant. These figures highlight the pressing need for increased awareness and proactive screening, as the study also found that the prevalence of HPV-16 was alarmingly high among participants, suggesting a direct link to lifestyle factors such as alcohol consumption and sexual practices.
The challenge posed by oral HPV cannot be overstated. As the data illustrates an unnerving rise in oropharyngeal cancers among men, particularly with HPV’s prevalence remaining constant regardless of age, a shift in vaccination strategy is warranted. Health authorities must not only promote the importance of HPV vaccination among younger populations but also expand efforts to include older demographics. A well-rounded approach will require focused public health initiatives, awareness campaigns, and potentially revised guidelines that recognize the unique risks faced by men. Only through vigilant action can we mitigate the potential ramifications of oral HPV and its associated cancers on a global scale.