For far too long, the dialogue surrounding menstruation has been relegated to whispers in the societal corridors of shame and stigma. However, groundbreaking research led by neuroscientists Elizabeth Rizor and Viktoriya Babenko at the University of California, Santa Barbara, is emerging as a beacon of insight. Their recent study illustrates the profound interplay between the cyclical shifts of hormones during the menstrual cycle and the intricate architecture of the human brain. It shines a light on an aspect of women’s health that has remained shrouded in mystery, highlighting the need for an expanded understanding of menstruation and its multifaceted effects on the brain.
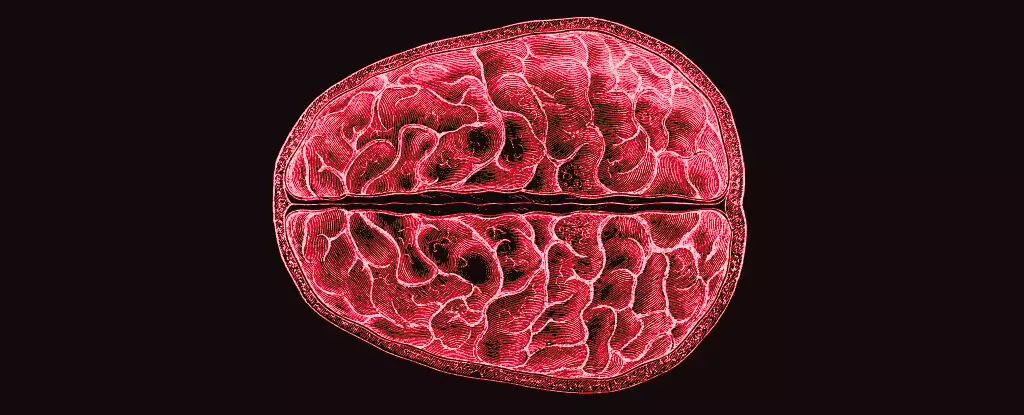
The study involved a methodical investigation of thirty women over the course of their menstrual cycles, integrating advanced imaging techniques, such as MRI scans, to capture real-time cerebral changes against the backdrop of hormonal fluctuations. As menstrual cycles unfold—spanning approximately 450 iterations over the typical lifespan—the interplay between ovarian hormones and brain structure is a captivating and critical area for exploration. Instead of merely cataloging the effects of hormones on mood or cognitive tasks, this research redirects the focus to the very fabric of the brain, challenging previous narratives and prompting a deeper inquiry.
Decoding Hormonal Fluctuations: A Structural Revolution
The findings from Rizor and Babenko’s study reveal that the influence of hormones permeates beyond the traditional boundaries of the hypothalamic-pituitary-gonadal (HPG) axis, suggesting that significant brain-wide changes may occur throughout various regions in the brain. The study concludes that structural modifications in both white and gray matter depend heavily on the menstrual cycle stage; specifically, the effects of estradiol and progesterone trigger observable transformations. These revelations push the boundaries of existing knowledge, with researchers stating, “These results are the first to report simultaneous brain-wide changes in human white matter microstructure and cortical thickness coinciding with menstrual cycle-driven hormone rhythms.”
By meticulously mapping the brain’s structural dynamics during menses, ovulation, and the mid-luteal phase, the researchers identified noteworthy correlations between hormonal peaks and alterations in brain anatomy. For instance, just prior to ovulation, surges in estradiol and luteinizing hormone were associated with changes in white matter that indicated accelerated information processing capabilities. Such findings invite further speculation on how these changes may affect cognitive function, emotional regulation, and even overall mental well-being.
The Need for Comprehension: Addressing the Menstrual Knowledge Gap
Despite the critical implications outlined in this study, the broader landscape of research on menstruation, especially in relation to neurological outcomes, remains largely underexplored. It’s perplexing, considering the biological reality affecting half the population for a significant portion of their lives. Traditional academic narratives have often overlooked the neurobiological implications of menstruation, focusing instead on cognitive performance during specific tasks without considering structural changes—a puzzling oversight.
Researchers assert the powerful behavioral and functional effects of hormonal fluctuations, yet, as Rizor, Babenko, and their colleagues poignantly noted, little is understood regarding how these hormonal changes can reshape the very wiring of the brain. Such ambiguity can have tangible repercussions; undefined mental health issues during menstruation, often trivialized or marginalized, may find their roots in these structural variances within the brain.
Setting the Stage for Future Discoveries
Rizor and Babenko’s work paves the way for future inquiries into the intimate relationship between women’s hormonal cycles and brain physiology. It raises compelling questions surrounding implications for mental health, particularly concerning severe period-related challenges that some women face. Understanding these neurological processes could not only enhance our approach to treatment but also inform broader conversations about both reproductive health and psychiatric care.
In a society struggling to adapt its understanding of menstruation, fueling childlike curiosity and rigorous examination is paramount. These findings beckon for further exploration, encouraging both the scientific community and the general populace to dismantle archaic narratives surrounding menstruation. Only through continued inquiry can we hope to unlock the transformative potential buried under layers of stigma and ignorance, recontextualizing menstruation from a mere biological process to an intricate orchestra of bodily and cognitive symphonies.