As the human body ages, its biological functions undergo profound transformations that significantly influence health outcomes, particularly concerning cancer risk. The relationship between aging and cancer is multifaceted and counterintuitive; while the risk of developing cancer typically escalates in the 60s and 70s, this trend intriguingly shifts after the age of 80. Recent research has begun to unravel the mechanisms that might explain this phenomenon, shedding light on the interplay between stem cell behavior, iron metabolism, and cancer.
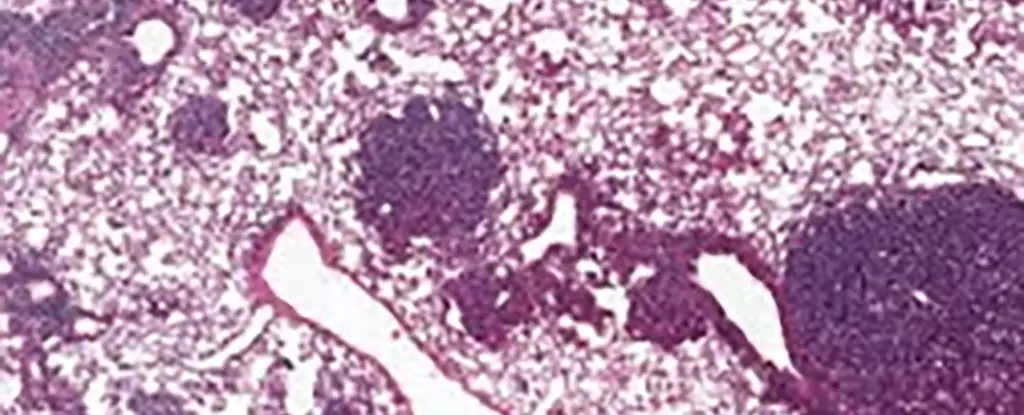
One striking observation in cancer epidemiology is the decline in cancer risk after reaching the age of 80. This perplexing pattern invites scrutiny into the biological underpinnings that characterize elderly populations. At the heart of understanding this decline lies the behavior of specialized lung cells known as alveolar type 2 (AT2) stem cells, crucial for lung regeneration and implicated in various lung cancers.
Studies conducted by international scientists, including a notable team from Memorial Sloan Kettering Cancer Center, reveal that older mice exhibit heightened levels of a protein named NUPR1. This protein seems to induce a cellular environment that mimics iron deficiency, despite the actual iron levels being abundant. Xueqian Zhuang, a cancer biologist, elaborates on this paradox: “Aging cells lose their capacity for renewal and therefore for the runaway growth that happens in cancer.” In essence, this limitation on cellular renewal processes reduces the opportunities for cancerous growth, signifying a potential biological mechanism for the decrease in cancer incidence among the elderly.
The research further demonstrated that NUPR1’s overexpression correlates with an effective reduction in iron availability for cellular functions. Intriguingly, when levels of NUPR1 are artificially reduced or when iron availability is increased, the regeneration capacity of the cells is significantly enhanced. This insight opens promising avenues for therapeutic exploration, particularly in targeting iron metabolism in older patients—an area of increasing interest amidst the long-term respiratory complications stemming from COVID-19.
Understanding how to harness the regenerative potential of AT2 cells could provide critical insights into improving lung health in older adults. With the aging population at the forefront of healthcare challenges, this research presents an opportunity to refine treatment protocols and enhance quality of life via targeted therapies.
The findings regarding NUPR1 not only advocate for a greater understanding of aging but also highlight the necessity of timing in cancer intervention strategies. The research elucidates that ferroptosis, an iron-dependent cell death mechanism, remains less prevalent in aging cells due to their functional deficiency in iron. This diminished susceptibility to iron-triggered cell death may necessitate earlier intervention with ferroptosis-based treatments to maximize their effectiveness.
As Tuomas Tammela points out, the implications for cancer prevention extend even to younger populations. Preventative measures against activities known to elevate cancer risk—such as smoking or excessive sun exposure—take on enhanced significance in light of these findings. The data suggest that the carcinogenic activities encountered during youth may pose more severe risks than previously acknowledged, marking a need for intensified public health initiatives targeting younger demographics.
The interplay of age, genetic predisposition, and environmental factors reveals a complex framework that clinicians must navigate in treating cancer. As Zhuang aptly notes, “There’s still a lot that’s unknown about how aging actually changes the biology of cancer.” This motivates the scientific community to further explore the implications of NUPR1 and its effects on both healthy cell regeneration and pathological growth.
The study of how aging influences cancer risk through mechanisms like NUPR1 and iron metabolism is still in its infancy. The potential for personalized treatment strategies that consider age-related factors marks an important frontier in oncology. As we continue to dissect the intricate relationships between aging and cancer, one thing remains clear: fostering a greater understanding of these processes is essential to advance cancer treatment and prevention, ultimately serving to improve health outcomes across all ages.