Mitochondria have long been stereotyped as mere cellular power plants, tirelessly churning out the energy that fuels biological processes. However, this traditional viewpoint underappreciates the sophisticated roles these organelles play, particularly in regulating immune functions. Recent scientific revelations highlight mitochondria as pivotal players in more than just energy metabolism—they also act as critical sentinels within immune cells, orchestrating responses that protect the body against bacterial invaders. This emerging perspective forces us to rethink how cellular metabolism intertwines with immunity and challenges the old, limited narrative about mitochondrial function.
The Unsung Role of Neutrophils and NETs
Among the frontline defenders of the immune system are neutrophils, the most abundant type of white blood cell. Their ability to rapidly respond to infection and contain microbial threats underpins our body’s initial defense strategy. One of their remarkable weapons is the formation of neutrophil extracellular traps (NETs): web-like meshes composed of DNA and antimicrobial proteins that ensnare and neutralize pathogens. Historically, NET formation was attributed predominantly to stressed or damaged cells signaling for a defensive response. Yet, this explanation feels too simplistic and overlooks the complexity underpinning immune activation.
Mitochondria as Metabolic Sensors Triggering Immune Action
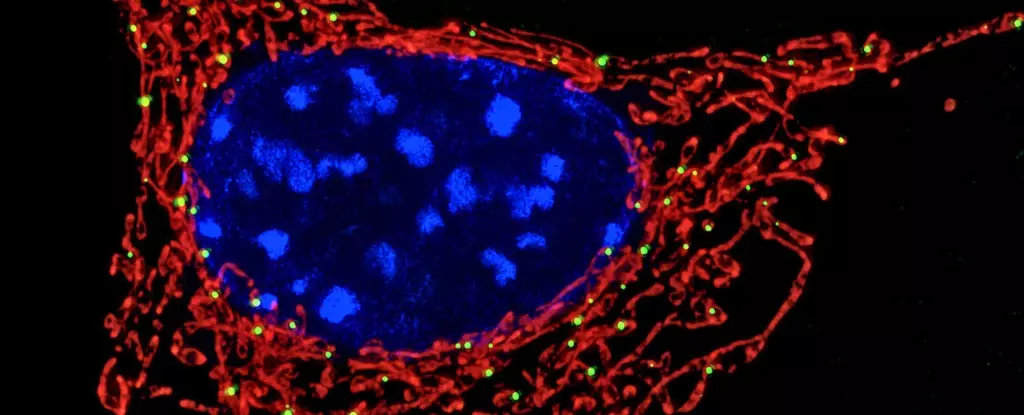
Groundbreaking research has unveiled an unexpected communication channel between mitochondria and bacterial metabolism. The discovery that mitochondria within neutrophils can detect lactate—a byproduct expelled by bacteria during their energy production—marks a paradigm shift. Instead of passively reacting to damage, mitochondria actively sense the metabolic whispers of bacteria trapped inside phagosomes, compartments within immune cells designed to engulf pathogens.
This sensing mechanism initiates NET production, effectively turning mitochondria into molecular spotters that can “smell” danger through bacterial metabolic footprints. This is an extraordinary feat given that lactate resides in a segregated intracellular compartment, far from where mitochondria typically operate. The mitochondria’s ability to pick up these localized cues reflects an intricate level of cellular coordination previously underappreciated in immunology.
The Mitochondria-Lactate Axis and Immune Dysfunction in Autoimmunity
The implications of this discovery extend beyond basic biology and offer critical insights into complex diseases such as systemic lupus erythematosus (SLE). SLE patients famously face a paradox: their immune systems are hyperactive and mistakenly attack their own tissues, yet they struggle to fend off infections. This contradiction has puzzled scientists, but the newfound understanding of mitochondrial signaling helps explain why.
In lupus, mitochondria appear dysfunctional, failing to recognize bacterial lactate efficiently. Consequently, the neutrophils in these patients produce fewer NETs, resulting in impaired bacterial trapping and destruction. This duality—excessive immune activation alongside compromised defense—underscores mitochondria’s role as balanced coordinators of immune responses. Their failure manifests both in unchecked autoimmunity and vulnerability to infection.
Reimagining Immunometabolism: Therapeutic Prospects
The acknowledgment that immune function and metabolism are inseparable opens fertile ground for therapeutic innovation. By enhancing mitochondrial sensitivity to bacterial signals, we might boost immune defenses in vulnerable populations, such as those suffering from lupus or immunodeficient states. Conversely, in conditions characterized by harmful overproduction of NETs—seen in severe COVID-19 or certain autoimmune pathologies—targeting mitochondrial pathways may allow us to temper excessive inflammation and tissue damage.
This nuanced approach could circumvent one-size-fits-all treatments that indiscriminately suppress or activate immune responses, instead offering precision interventions that recalibrate immune cell metabolism to desirable states.
Looking Ahead: Expanding the Mitochondrial Frontier
While the focus thus far has been on neutrophils, it’s reasonable to hypothesize that other immune cell types might exploit similar mitochondrial sensing mechanisms, responding to diverse microbial metabolites beyond lactate. If confirmed, this would suggest a universal model where mitochondria act as hubs deciphering microbial metabolic cues to fine-tune immunity.
Unlocking these pathways in richer detail could revolutionize how we understand infections, autoimmunity, and inflammation. It evocatively positions mitochondria not just as the “powerhouses” of cells but as vigilant sentinels—dynamic organelles capable of orchestrating complex immune decision-making. Appreciating this dual function challenges researchers and clinicians alike to reconsider mitochondrial biology’s centrality in health and disease, arguably setting the stage for a transformative era in immunological research and therapeutic strategy.