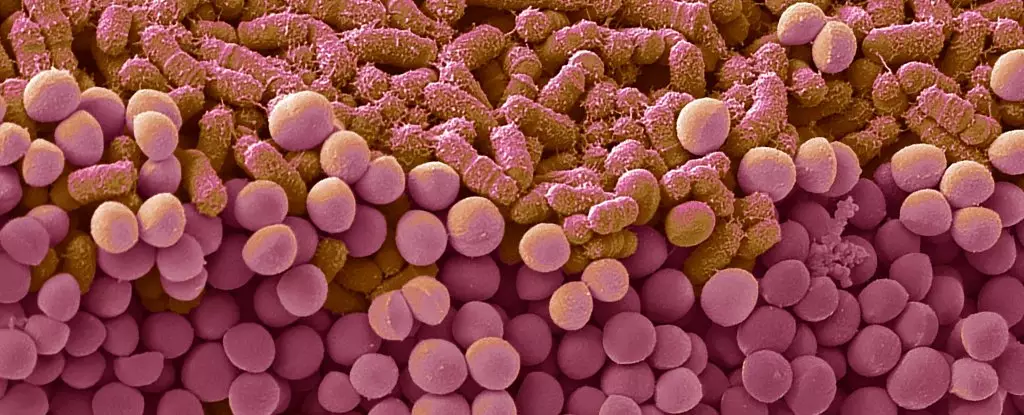
In the relentless pursuit of weight loss, many individuals unwittingly fall into a frustrating cycle known as yo-yo dieting, where repeated cycles of restrictive dieting followed by overeating undermine long-term success. A groundbreaking study from French researchers propels our understanding of this phenomenon into a new realm—the microscopic universe within our gut. Far from being passive passengers in our digestive system, gut bacteria play a pivotal role in shaping our cravings, mood, and even our propensity for binge eating. The intricate dance between diet, microbiome composition, and brain function suggests that the key to sustained weight management could lie in manipulating these unseen microbial communities.
This research challenges the conventional focus solely on calorie counting and willpower. Instead, it uncovers how oscillations between healthy and unhealthy eating patterns leave a lasting imprint on the microbiome. The consequences are profound: not only do these shifts thwart future dieting efforts, but they may actively drive the disordered eating behaviors that make weight loss so elusive. This paradigm shift urges us to think of diet interventions as complex biological exchanges rather than merely behavioral choices.
How Diet Cycles Remodel Our Microbiome and Brain Function
The study’s core insight reveals that alternating between nutrient-rich and calorie-dense, sugar-laden diets causes persistent changes to gut bacteria. When mice underwent diet swings between standard and high-fat, high-sugar regimes, they developed an increased hedonic drive—an intensified attraction to pleasurable eating—after returning to healthier diets. This suggests a biological rewiring, akin to a craving circuit being reconfigured by fluctuating diets.
Remarkably, the research demonstrated causality: transferring the altered microbiome from diet-cycled mice into those with no prior dieting experience induced similar binge-eating behaviors. This indicates that the microbiome itself, once reshaped, can directly influence food reward systems in the brain, rewiring the neural pathways that differentiate between hunger and craving. The findings imply that yo-yo dieting does more than temporarily sabotage weight goals; it actively transforms our internal biology in ways that make healthy choices more difficult, creating a vicious cycle of craving and overeating.
This points to a disturbing yet fascinating possibility—our gut bacteria might hold the blueprint for our food addictions. If so, disrupting this microbial influence could open new pathways for interrupting binge episodes and establishing lasting dietary habits. But it also complicates existing weight-loss strategies, highlighting that addressing only calorie deficits may overlook a crucial biological driver.
Implications for Future Research: Personalized Treatments and Microbial Targets
While these results are compelling, they inevitably raise questions about their applicability to humans. Nevertheless, the implications are enough to warrant immediate attention. If dietary fluctuations engender microbiome alterations that promote overeating, then stable, consistent eating patterns might be vital not just for caloric balance but for microbiome stability—serving as a biological foundation for lasting change.
The next frontier involves identifying specific bacterial species or functional pathways involved in this process. Could probiotic treatments or microbiota-targeted therapies dampen the urge to binge after dieting? Might we develop tailored interventions that reshape the gut microbiome into a state resistant to the rewiring caused by diet cycles? Such approaches could revolutionize weight management, transforming it from a matter of willpower into a finely tuned biological strategy.
Furthermore, future research must extend beyond animal models to human trials. Our complex social, psychological, and environmental factors intersect with gut microbiota, making the picture more tangled yet more promising. Personalized microbiome profiling could become a standard aspect of weight management, helping clinicians design diets that foster microbial communities supportive of sustainable habits rather than destructive cycles.
A Paradigm Shift in How We View Diet and Health
This research compels us to rethink dieting itself—not as a purely behavioral challenge but as a biological one as well. The microbiome emerges as a central player in the maintenance of weight and healthy eating patterns, capable of tipping the scales in either direction. It urges the health community to develop holistic, microbiome-centered strategies rooted in an understanding that our internal microbial ecosystem is both a mirror and a master of our eating behaviors.
The power inherent in this discovery lies in its potential to redefine the mental and physiological hurdles that sabotage dieting efforts. Instead of merely fighting cravings, we might learn to recalibrate the microbial environment that fuels them. The journey toward healthier, more resilient bodies might therefore hinge on harnessing, nurturing, and even rewiring our gut bacteria, making them allies rather than adversaries in the fight against obesity.