The relationship between breast cancer survival and Alzheimer’s disease risk opens a fascinating chapter in the complex narrative of how different health challenges intersect. Traditionally, cancer treatments—especially chemotherapy—have been closely associated with cognitive decline, a phenomenon often called “chemobrain.” It’s commonly believed that the rigors of cancer therapy leave survivors vulnerable to memory lapses, difficulty concentrating, and other neurological issues. However, recent insights challenge this assumption by suggesting that breast cancer survivors might actually experience a modest reduction in Alzheimer’s risk, raising critical questions about the long-term neurocognitive consequences of cancer treatment.
A Closer Look at the Evidence
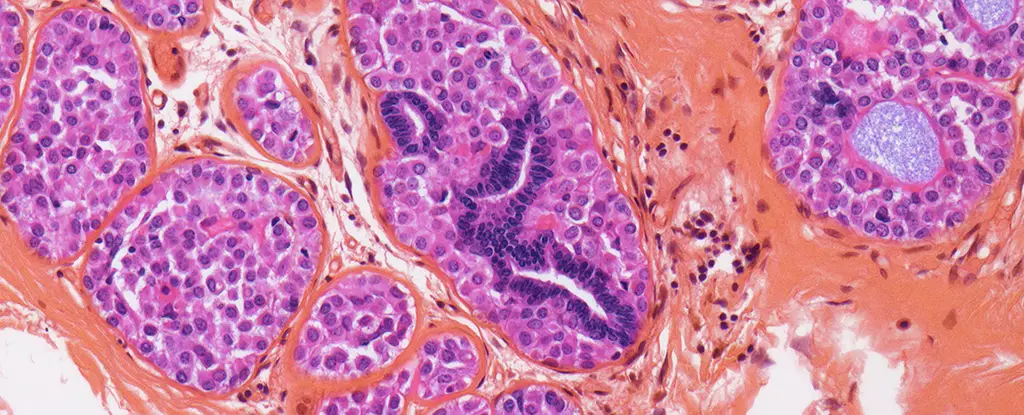
The new research, conducted in South Korea and involving over 70,000 breast cancer patients compared with upwards of 180,000 healthy controls, detected an 8% lower incidence of Alzheimer’s disease among the survivors during an average follow-up of 7.3 years. While an 8% difference may appear subtle at first glance, it takes on significance in the context of public health, especially among women over 65, where Alzheimer’s cases naturally rise. This protective signal also seemed strongest among those treated with radiation therapy, and intriguingly, the risk reduction diminished as time passed. This temporal pattern suggests that cancer therapies might exert biological effects beyond tumor control—effects that could influence brain pathology in ways not yet fully decoded.
The Contested Role of Radiation Therapy
Radiation therapy has long been recognized for its destructive capacity directed at malignant cells, but its impact on surrounding tissues, especially the brain, remains less understood. Emerging evidence hints that radiation may reduce neuroinflammation, a recognized driver of Alzheimer’s pathology. By possibly dampening inflammatory processes, radiation might confer an unforeseen neuroprotective benefit. Still, this hypothesis remains speculative, and the observational nature of the data prevents us from establishing direct causality. The decrease in Alzheimer’s risk among breast cancer survivors, particularly those receiving radiation, should encourage rigorous mechanistic studies to unravel these complex biological interactions.
Challenging Prevailing Assumptions About Chemobrain
Contrary to the widely reported cognitive impairments during and shortly after cancer treatment, the new evidence implies that these cognitive challenges do not necessarily translate into an increased risk of Alzheimer’s disease—a distinction of paramount importance for patients, caregivers, and clinicians alike. Chemobrain might reflect transient or reversible disruptions rather than the progressive neurodegeneration characteristic of Alzheimer’s. This calls for a nuanced understanding of cognitive sequelae post-cancer treatment and an urgent need to separate immediate cognitive side effects from long-term neurodegenerative risks.
Implications for Survivorship and Future Research
With survival rates for breast cancer steadily improving—largely due to advances in early detection and treatment—there is a growing population of women living with the long-term consequences of cancer and its therapy. Understanding how these treatments impact brain health and Alzheimer’s risk is critical for patient counseling, management, and monitoring. This research underscores the complexity of survivorship, emphasizing that therapy-related cognitive concerns should not overshadow the potential neuroprotective effects that may arise unexpectedly.
These findings also spotlight the broader question of how immune modulation and systemic inflammation—common threads in both cancer and neurodegeneration—interact. The idea that treatments reducing systemic or brain inflammation during cancer therapy might incidentally lower Alzheimer’s risk is provocative and opens new avenues for interdisciplinary research that intersects oncology with neurology and immunology.
Looking Beyond Statistics to Real-World Impact
While this study’s statistical significance is compelling, translating these findings into clinical practice requires careful interpretation. For instance, the 8% reduction, while modest, could represent meaningful protection given Alzheimer’s high prevalence. However, individual risk factors such as genetics, lifestyle, and comorbidities will still dominate Alzheimer’s risk profiles. It’s critical to frame this knowledge not as a simple ‘silver lining’ of cancer survival, but as a starting point for deeper investigations into how cancer biology and treatments influence brain aging.
In my view, this emerging evidence encourages a shift from viewing cancer treatments as purely harmful to cognitive health to considering their nuanced, sometimes paradoxical, effects. It invites optimism about potential protective mechanisms locked within treatment responses and compels the medical community to rethink cancer survivorship beyond tumor eradication—towards holistic long-term brain health.