Recent developments in the treatment of Alzheimer’s disease, particularly with the introduction of the drug lecanemab, offer glimmers of hope for delaying cognitive decline in patients. In a groundbreaking phase 3 clinical trial, lecanemab demonstrated a noteworthy ability to slow cognitive decline by up to 27 percent compared to a placebo. This finding led to the drug’s approval by the FDA in 2023, enabling a much-needed therapeutic option for those struggling with this debilitating condition.
However, as promising as these results are, new analyses indicate a concerning disparity in how male and female patients respond to lecanemab. While the results for men indicate a significant 43 percent slowing of cognitive decline, female subjects reported a meager 12 percent improvement—a discrepancy of nearly 31 percent. Given that two-thirds of Alzheimer’s patients are women, these findings illuminate a substantial gap in efficacy that must not be overlooked.
The Need for Gender-Sensitive Research
The lack of comparable data between male and female participants in clinical trials highlights a critical oversight in medical research. The preliminary results, while encouraging, require further examination to ensure that all demographic groups benefit equally from advancements in treatment. Neuroscientist Marina Lynch, from Trinity College Dublin, criticized the decades of research that often ignored sex as a potential influencing factor. “Until relatively recently, recruitment for clinical trials did not give due consideration to the possible impact of sex on outcomes,” she lamented.
In response to this ongoing issue, researchers from Canada and Italy conducted a series of simulations based on clinical data from the CLARITY AD trial. These simulations revealed that the difference in drug efficacy observed between sexes might be more random than systematically tied to biological factors. Even so, the known differences in brain aging processes between men and women only account for a fraction of the observed discrepancy.
The Mysterious Mechanisms of Amyloid Clearing
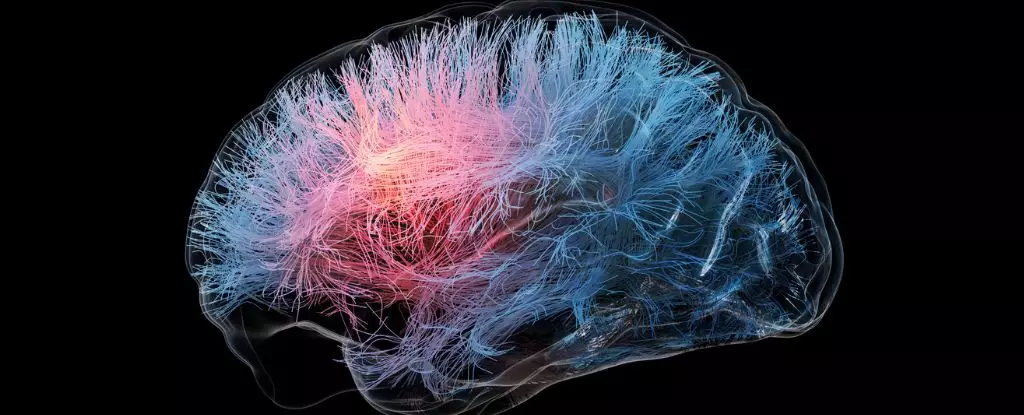
Lecanemab operates by targeting amyloid plaques in the brain, long regarded as a major contributor to Alzheimer’s pathology. Despite the drug’s success in some patients, it remains unclear how effectively and uniformly it operates across different demographics. For decades, amyloid plaques have been championed as the harbingers of dementia, but emerging research suggests that the relationship is far more complex. There exist patients who, despite having notable cognitive decline, exhibit a complete absence of these plaques in postmortem examinations.
This raises crucial questions regarding the proposed mechanisms of amyloid-targeting treatments like lecanemab. If nearly a third of diagnosed Alzheimer’s patients do not present with amyloid plaques, reliance on such targets becomes increasingly tenuous. Furthermore, the potential influence of sex chromosomes and hormones complicates the situation further, suggesting that drug responses may vary considerably between men and women. Current evidence indicates that certain drugs may engage with amyloid in distinctly different ways depending on the patient’s sex.
The Call for Revolution in Research Protocols
The academic community is beginning to recognize the dire consequences of neglecting these gender disparities in Alzheimer’s research. The alarming assertion from an international coalition of scientists warns of a “disproportionate burden” placed on women’s health and well-being due to a persistent “male bias” in brain aging studies. This bias not only limits the understanding of Alzheimer’s disease but also prolongs the suffering of countless individuals who might otherwise benefit from more effective, gender-specific treatments.
The necessity for sex-disaggregated data in clinical trials has never been clearer. Identifying how treatments like lecanemab influence various demographic groups can reveal critical insights that might change the standard approach to diagnosing and managing Alzheimer’s. The ultimate goal is to develop personalized medicine that can more effectively address the unique needs of both men and women.
As the scientific landscape grows increasingly concerned with inclusivity, it remains essential for drug developers to share trial data in a manner that fosters collaborative exploration of these complex issues. By understanding the gendered dimensions of disease, researchers may uncover new treatment avenues, ultimately leading to improved health outcomes for millions worldwide.
In this ongoing journey towards effective Alzheimer’s therapies, addressing the gender gap is not merely a matter of scientific accuracy; it is a pressing ethical obligation to ensure equitable health care for all patients. We stand at a new frontier, where understanding the differences between male and female brains could fundamentally alter the landscape of Alzheimer’s treatment and care.